
The CPC was adapted from the Glasgow Outcome Scale (GOS) for traumatic head injury. CPC 1 corresponds to the best possible outcome (no or minor disabilities) while CPC 5 corresponds to death (Table 1). The most commonly used measure for reporting neurological outcome after CA is represented by Cerebral Performance Categories (CPCs).
#Unequal pupil size after a heart attack how to
The aims of the present review are to summarise the current knowledge on the prediction of neurological outcome in patients who are comatose after CA and to provide practical recommendations on how to perform an accurate neuroprognostication in these patients. The characteristics of these categories of predictors are discussed in this article. These may include clinical neurological examination, electrophysiological investigations (electroencephalogram (EEG) and short-latency somatosensory evoked potentials (SSEP)), serum biomarkers, and neuroimaging. However, even the most robust neurological predictors are not 100% specific for this reason, the current guidelines recommend using a combination of predictors.

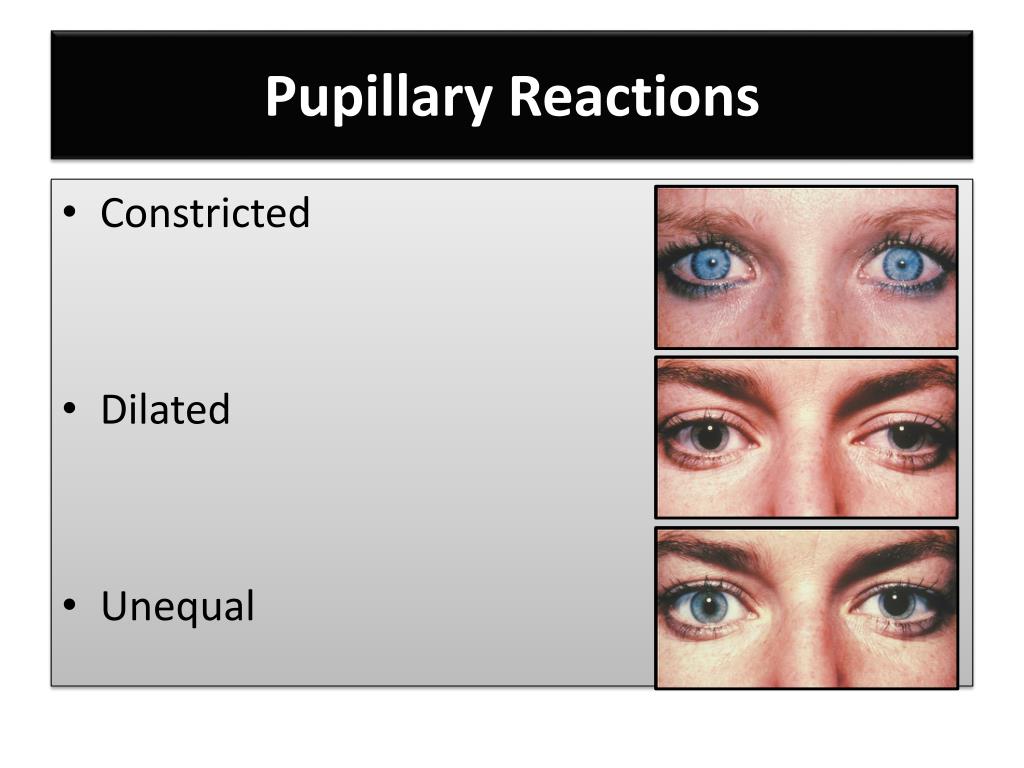
the ratio between the number of patients with a falsely pessimistic prediction divided by the number of patients with good neurological outcome) of the index used should ideally be zero, or their specificity should be 100%. In other words, when predicting a poor neurological outcome, the false positive rate (FPR) (i.e. To avoid premature WLST in patients with a chance of neurological recovery, the risk of a falsely pessimistic prediction should be kept to a minimum. In fact, most deaths caused by HIBI result from withdrawal of life-sustaining treatment (WLST) following prognostication of a poor neurological outcome. However, only a minority of these deaths occur as a direct consequence of massive neuronal injury (i.e. Severe HIBI causes delayed neuronal death and diffuse brain oedema. A multimodal approach combining multiple prognostication tests is recommended so that the risk of a falsely pessimistic prediction is minimised.Ībout 80% of patients who are admitted to an intensive care unit (ICU) after resuscitation from out-of-hospital cardiac arrest (OHCA) are comatose and two thirds of them will die because of hypoxic–ischaemic brain injury (HIBI). Current guidelines recommend performing prognostication no earlier than 72 h after return of spontaneous circulation in all comatose patients with an absent or extensor motor response to pain, after having excluded confounders such as residual sedation that may interfere with clinical examination. The most commonly used indicators of severe HIBI include bilateral absence of corneal and pupillary reflexes, bilateral absence of N 2O waves of short-latency somatosensory evoked potentials, high blood concentrations of neuron specific enolase, unfavourable patterns on electroencephalogram, and signs of diffuse HIBI on computed tomography or magnetic resonance imaging of the brain.
A poor neurological outcome-defined as death from neurological cause, persistent vegetative state, or severe neurological disability-can be predicted in these patients by assessing the severity of HIBI. Hypoxic–ischaemic brain injury (HIBI) is the main cause of death in patients who are comatose after resuscitation from cardiac arrest.


 0 kommentar(er)
0 kommentar(er)
